All fields are required
Posted in Outbreaks & Recalls on July 14, 2024

In the last 30 days, the U.S. Food and Drug Administration (FDA) has announced two Salmonella outbreaks with no source identified. Both outbreaks are in the traceback investigation process. The investigations are ongoing.
Here’s what we know.
The FDA identified a cluster of Salmonella Typhimurium illnesses and initiated an outbreak investigation on June 19, 2024. The case count recently increased from 80 to 83 linked cases.
While traceback investigation activities have been initiated to determine the source of the outbreak, no product has been confirmed as a likely source of the illnesses.
This week another cluster of Salmonella illnesses, this time with the Salmonella Irumu strain, was identified. This prompted a second Salmonella outbreak investigation on July 10, 2024.
So far there are 26 linked illnesses in this Salmonella Irumu outbreak. Traceback investigation activities have been initiated. However, no source has been identified at this time.
These two Salmonella outbreaks do not have an identified food source. Any food could potentially become cross-contaminated with harmful Salmonella bacteria. However, certain foods have a stronger association with this bad bug than others.
While not a conclusive list of potential suspects, the following foods have been identified in previous Salmonella outbreaks over the last five years.
Just in the last five years, Salmonella Typhimurium outbreaks have made an appearance many times. From the recent outbreak linked to fresh basil to alfalfa sprouts to prepackaged salads.
Looking even further back, this Salmonella strain has been linked to dried coconut and chicken salad in 2018, ground beef in 2013, cantaloupe in 2012, again in ground beef in 2011, peanut butter in 2009, and in tomatoes in 2006 as the earliest documented Salmonella outbreak on the FDA’s Salmonella outbreak page.
Salmonella Irumu did not come up once.
Prevention is key. Though foodborne illness is sometimes unavoidable, taking a few extra precautions could make a huge difference.
This is the most important step in preventing illness. Wash your hands before preparing food or eating. Wash you hands after using the restroom or helping someone use the restroom (including changing diapers). Also, wash your hands after handling animals or being in areas where they live.
Separate raw foods from cooked or ready to eat foods at every step of the process. While in your cart in the grocery store to the bags at checkout, to storage at home. Never place cooked food on a surface that raw meat has touched and thoroughly clean utensils and plates after contact with raw food.
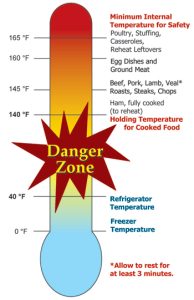
Always cook food to a safe internal temperature. Use an instant read food thermometer for best results. Follow the USDA guidelines for these guidelines. This information can be found on the U.S. Department of Agriculture’s Safe Minimum Internal Temperature Chart.
If you do become infected by Salmonella bacteria, you are not alone. The Centers for Disease Control and Prevention (CDC) estimates that around 1.35 million infections, 26,500 hospitalizations, and around 420 deaths are attributed to Salmonella bacteria in the United States each year. Food is the most common source of these illnesses.
If exposed, your symptoms may start anywhere from six hours to six days.
Common symptoms include diarrhea (sometimes bloody), fever, and/or stomach cramps. Some people may also experience nausea, vomiting, or a headache.
For most normally healthy individuals, these symptoms may resolve on their own without medical intervention within four to seven days.
Others may not be so lucky. Some groups of people are more likely to become infected if exposed or experience more serious illness if infected. These are considered higher risk groups.
Children under 5 years old and people taking certain medications, such as stomach acid reducers, are at higher risk of infection if exposed. Infants, individuals over 65 years, and those with a weakened immune system are more likely to experience severe infections.
In most cases, no treatment is necessary to recover from Salmonella infection. Antibiotic treatment can be used in those at higher risk but are reserved for extreme circumstances to reduce the incidence of antibiotic resistance.
Hydration and rest are key elements of Salmonella infection recovery. Replacing lost fluids from vomiting and diarrhea can help you feel better faster.
In some cases, you will want to seek medical care. If illness becomes severe, you become dehydrated, or experience complications, reach out to your healthcare provider.
Call the doctor if you have:
These could be signs of sever infection or complications. Other complications may include Reactive Arthritis (resulting in painful urination, eye irritation, and joint pain), blood infections, or infections throughout the body such as meningitis, heart complications, and long-lasting disruptions of bowel habits.
If you believe you have become sick with Salmonella Illness and may be associated with these outbreaks, there are a few things you can do to help your situation.
First, reach out to your healthcare provider or local health department. Determining the cause of your illness and associating the strain of bacteria with a cluster of illnesses can help investigators track down the cause of the outbreak.
Stay hydrated! Dehydration is a serious concern during foodborne illness.
Get advice from an experienced Salmonella lawyer. Lost wages, medical bills, and other burdens associated with foodborne illness can add up quickly. Get advice to find out if you have a legal case.
The Lange Law Firm, PLLC has experience representing cases just like yours. Call (833) 330-3663 or click here for a free consultation to go over the details of your situation. Don’t wait to get the help you deserve!
By: Heather Van Tassell (contributing writer, non-lawyer)